
white fillings
‘compacted tooth-coloured material used to occupy a cavity or space’
a dental filling is used to replace part of a tooth that has been lost either through neglect, lifestyle or accidental damage. the most common reasons for needing a filling are
tooth decay
 the most common cause of fillings. plaque forms when bacteria feed on the sugars and starches left on your teeth by food or drink. the acids in plaque soften and dissolve tooth enamel , causing tiny holes which then grow bigger and lead to sensitivity and pain,
the most common cause of fillings. plaque forms when bacteria feed on the sugars and starches left on your teeth by food or drink. the acids in plaque soften and dissolve tooth enamel , causing tiny holes which then grow bigger and lead to sensitivity and pain,
acid erosion
the protective enamel coating of teeth can get worn away by acids in certain foods and drinks or with some medical conditions like reflux or hiatus hernia.
cracks/chips
broken or chipped teeth usually result from injury, or after eating something very hard.
this in turn may expose the inner parts of the tooth and lead to erosion over time.
abrasion/attrition
teeth will wear over time, perhaps through aggressive toothbrushing or tooth grinding (bruxism).
there are 3 different types of white filling.
composite, glass ionomer and compomer.
composite restorations
 these are the most commonly placed white fillings.
these are the most commonly placed white fillings.
the resin is a versatile, clinically proven, successful and aesthetic material.
they are ‘direct’ restorations ie done on site.
the procedure is relatively quick and is one of the most cost-effective cosmetic dental procedures.
shades of composite are chosen to match the tooth colour.
to achieve a natural look typically two or more shades are chosen to build up the dentine and then the enamel shades as no tooth is one colour. the tooth near the gum is darker, whereas the area of the tooth at the biting surface is more translucent and lighter.
the composite is bonded to the tooth tissue with the recommended adhesive, hand sculpted into the desired shape, hardened and polished to achieve the best aesthetics.
glass ionomer restorations
the beneficial characteristic of this material is that it sticks to the tooth surface well and can also release fluoride which helps to strengthen the tooth tissue.
in deep restorations this filling may be placed underneath composite restorations to protect the nerve tissue and minimise the possibility of future problems, such as root canal treatment.
however it does not have the same aesthetics as composites and tends not to be as strong.
compomers
this material is a fusion of the above two materials. it is less commonly used but still has a place in some cases where aesthetics are required but strength is not as important.
pros
- to place a white filling requires less tooth to be drilled.
- they look great.
- they can be repaired as opposed to replaced.
cons
- they take longer to place.
- can be sensitive immediately after placement.
- will last for years, but not as long as a gold filling
inlays: crowns: bridges
all the above are ‘indirect restorations’. meaning that while the teeth are prepared and measured in the dental chair, impressions of the prepared teeth are sent to the dental technician who will prepare moulds and make the desired restoration in his laboratory. Typically the restorations are cast or fired in a kiln. They are much stronger than ‘direct’ restorations and therefore last a lot longer.
inlays
‘a filling shaped to fit a tooth cavity’
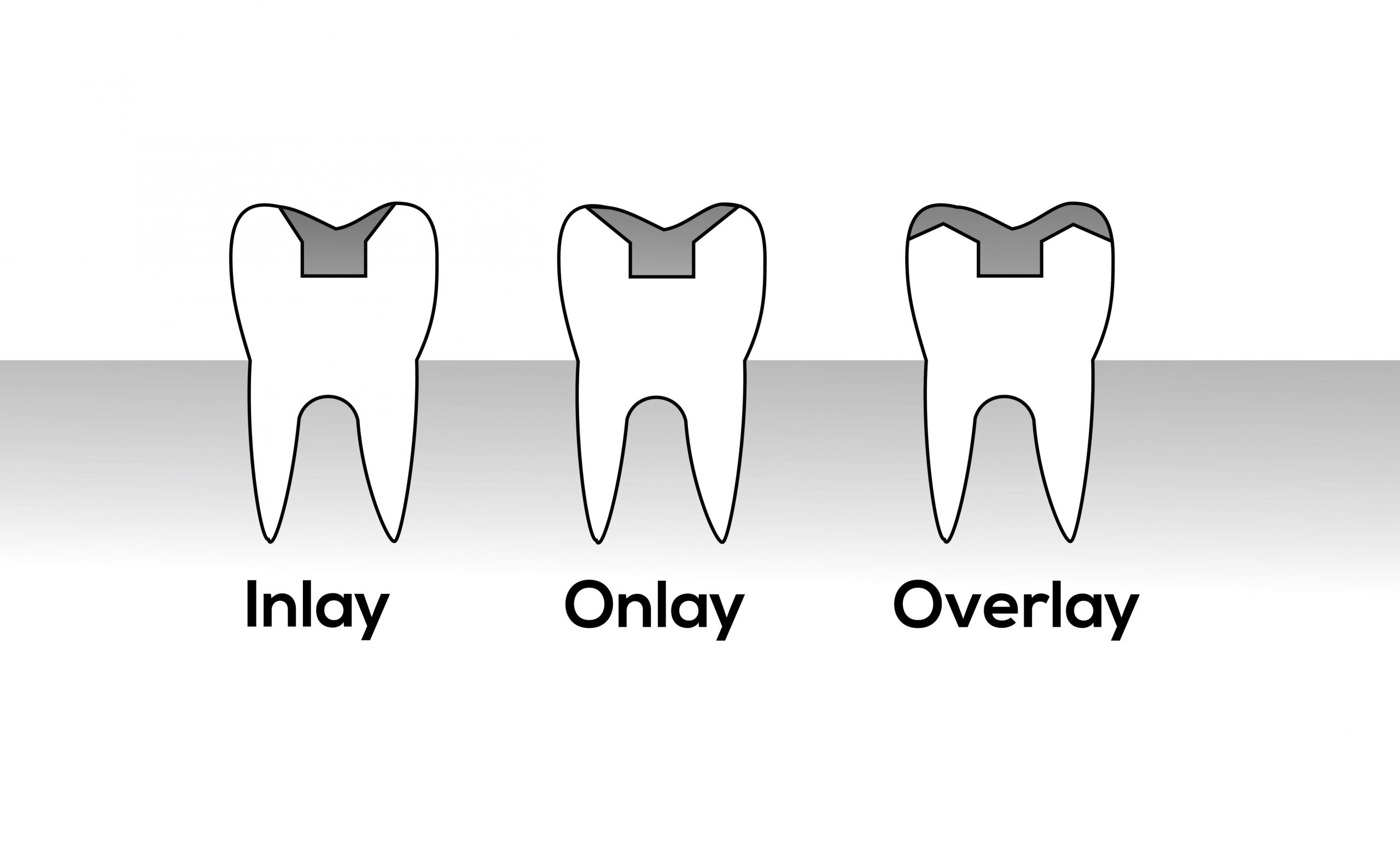 inlays provide an alternative to fillings, replacing part of a tooth that has been lost because of decay, wear or accidental damage. they are especially suitable for the chewing surfaces on back teeth. because of their increased strength they are particularly suited for larger cavities and for those who grind their teeth
inlays provide an alternative to fillings, replacing part of a tooth that has been lost because of decay, wear or accidental damage. they are especially suitable for the chewing surfaces on back teeth. because of their increased strength they are particularly suited for larger cavities and for those who grind their teeth
porcelain inlays
ceramics are perfect for restoration of the larger cavity. constructed in the lab, the porcelain is baked in a furnace. they are harder and stronger than the direct composite filling above, yet just as cosmetic.
gold inlays
again, made in the lab. gold is still the material of choice in restorative dentistry. extremely hard wearing and strong in thin section it has excellent finishing lines. it is a noble metal and therefore does not corrode when in saliva all day. a very wise and long-term choice. however, all dentists are ware that aesthetically it lets us down, especially when in the smile line.
crowns
‘an artificial substitute for the natural crown of the tooth’
 essentially a ‘jacket’ for the tooth.
essentially a ‘jacket’ for the tooth.
used to protect teeth that have been mechanically weakened by large fillings and root canal therapy, or by accidental fracture. they can also be used to correct smile lines and abrasion/erosion eg. from acidic overdose or grinding (bruxism). the crown serves to hold the remainder of the tooth and filling together, or replaces the fractured/worn tooth structure providing a durable, long-term restoration.
bridges
‘a fixed replacement for one or several absent teeth’
 a bridge is a fixed dental restoration used to replace a missing tooth (or several teeth) by joining an artificial tooth permanently to adjacent teeth or dental implants. they literally bridge the gap created by one or more missing teeth. it is made up of two or more crowns for the teeth on either side of the gap i.e. the abutment teeth, with a false tooth spanning the gap in-between.
a bridge is a fixed dental restoration used to replace a missing tooth (or several teeth) by joining an artificial tooth permanently to adjacent teeth or dental implants. they literally bridge the gap created by one or more missing teeth. it is made up of two or more crowns for the teeth on either side of the gap i.e. the abutment teeth, with a false tooth spanning the gap in-between.
root canal therapy
root canal therapy, also known as endodontic therapy, is a dental treatment for removing infection from inside a tooth. it can also protect the tooth from future infections.

root canals, and their associated pulp chamber, are the physical hollows within a healthy tooth that are naturally inhabited by nerve tissue, blood vessels and other cellular entities. together, these items constitute the dental pulp. decay or injury can destroy the living pulp. dead pulps lack a decent blood supply and are therefore more prone to infection leading to dental abcess and toothache.
endodontic therapy involves the removal of these structures, the subsequent shaping, cleaning, and decontamination of the hollows with small files and irrigating solutions, and the obturation (filling) of the decontaminated canals.
filling of the cleaned and decontaminated canals is done with an inert filling such as gutta-percha and typically a eugenol-based cement. endodontics includes both primary and secondary endodontic treatments as well as periradicular surgery which is generally used for teeth that still have potential for salvage.
when is root canal necessary?
if the pulp becomes injured or diseased, it cannot repair itself, and the tissue dies.
if a person has a deep cavity, a cracked tooth, or a loose filling, bacteria can enter the pulp. The bacteria will eventually destroy the pulp and if the bacteria penetrate through the root openings, this can cause an infection in the bone.
an infection will weaken the bone and break it down. the ligaments around the tooth will swell, and the tooth will become loose. a pulp injury will make the tooth very sensitive to high and low temperatures. there may be pain when chewing, and some people have a continuous, throbbing pain.
root canal therapy, extraction or implant?
without treatment, the infection will spread. eventually, the tooth will become loose and need extracting.
some patients may prefer to have the tooth pulled out, especially if it hurts a lot or if the tooth cannot be restored. this can happen if there is large decay, trauma, or loss of bone due to periodontal, or gum, disease.
be warned, removing a tooth may mean that the surrounding teeth start to move and become crooked. this not only looks unsightly, but can make it hard to bite properly.
root canal therapy will usually save the tooth and eliminate the pain.
if the tooth cannot be saved, the next best option is an implant, but it is better to save the natural tooth if possible, because nothing functions as well as a natural tooth.
root canal therapy complications
as with any surgery, sometimes complications can occur.
one problem is when the dentist only finds three root canals in a tooth that has four of them. if one canal remains untreated, the infection might continue and spread into the bone.
the dentist must also make sure the filling material goes far enough into the canal, to fill it up. if the root canal is not properly sealed, the infection could return.
during the procedure, the root of the tooth may crack, or instruments can break in the canal or perforate the canal. this makes it hard to fill the tooth effectively.
should complications occur, a specialist can try to correct the problem and complete the root canal. to avoid this, patients should always follow the dentist’s instructions. if an antibiotic is needed, it is important to finish the entire course.
it is essential to have a permanent restoration, such as a crown, placed once the root canal therapy is complete.
dental implants
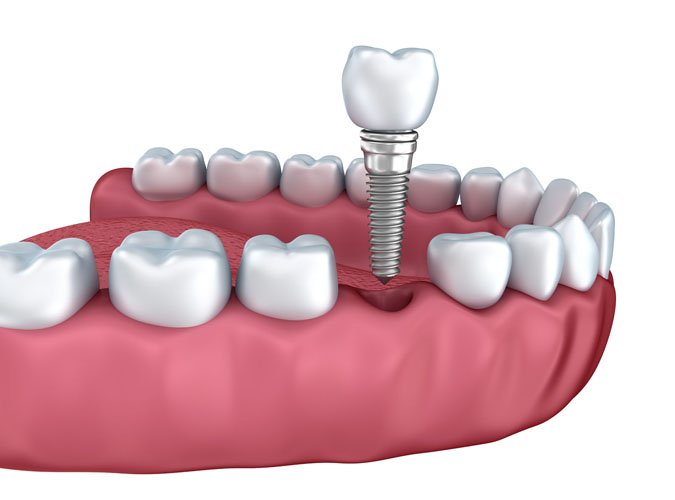
a dental implant (also known as an endosseous implant or fixture) is a surgical component that interfaces with the bone of the jaw or skull to support a dental prosthesis such as a crown, bridge, denture, facial prosthesis or to act as an orthodontic anchor.
they are used to replace missing teeth. typically made of titanium, implants are screws that are placed into the jaw bone. the bone then grows into the threads of the screw and becomes ‘fixed’ i.e. implanted. the process is known as osseointegration.
within aseptic surroundings, bone is exposed in the jaw where the tooth is missing. the screw is inserted into the bone and the gum is stitched over it. it is then left for 3 months to allow the bone to integrate with it. if the integration is successful a second procedure is planned when the implant is exposed and the surface structure is made to fit the implant.
 not everyone is suited for dental implants.the gums must be healthy and there must be adequate depth and width of jawbone to house the titanium screw, although techniques are available to add additional bone if needed. dental hygiene must be excellent and maintenance i.e. regular dental visits are essential. general health is an important factor too, diabetics and smokers, for example, are not candidates for successful dental implant work as healing is diminished and the osseointegration less likely to occur.
not everyone is suited for dental implants.the gums must be healthy and there must be adequate depth and width of jawbone to house the titanium screw, although techniques are available to add additional bone if needed. dental hygiene must be excellent and maintenance i.e. regular dental visits are essential. general health is an important factor too, diabetics and smokers, for example, are not candidates for successful dental implant work as healing is diminished and the osseointegration less likely to occur.
the technology is however, very, very clever indeed. whilst implants are still no substitute for ‘real’ teeth, they certainly have improved the quality of life, in terms of eating, speaking and aesthetics, for many, many people.
dentures
‘a removable plate or frame holding one or more artificial teeth’
often referred to as ‘false teeth’, dentures or plates are used to replace one or more missing teeth and the surrounding tissue. there are two types. partial dentures replace a few missing teeth, complete dentures replace all the natural teeth. they can be made wholly of acrylic, or acrylic and a light metal, such as cobalt chrome. the latter is more secure and less bulky but also more expensive.
complete dentures
 complete plates can be either “conventional” or “immediate.” made after the teeth have been removed and the gum tissue has begun to heal, a conventional plate is ready for placement in the mouth about eight to 12 weeks after the teeth have been removed
complete plates can be either “conventional” or “immediate.” made after the teeth have been removed and the gum tissue has begun to heal, a conventional plate is ready for placement in the mouth about eight to 12 weeks after the teeth have been removed
unlike conventionals, immediate dentures are made in advance and can be positioned as soon as the teeth are removed. as a result, the wearer does not have to be without teeth during the healing period. however, bones and gums shrink over time, especially during the healing period following tooth removal. therefore a disadvantage of immediates compared with conventionals is that they will require relining to fit properly during the healing process and generally should only be considered a temporary solution until conventional dentures can be made.
partial dentures
 a removable partial plate usually consists of replacement teeth attached to a pink or gum-colored plastic base, which is sometimes connected by metal framework that holds it in place in the mouth. partial plates are used when one or more natural teeth remain in the upper or lower jaw. not only does it fill in the spaces created by missing teeth, it prevents other teeth from changing position.
a removable partial plate usually consists of replacement teeth attached to a pink or gum-colored plastic base, which is sometimes connected by metal framework that holds it in place in the mouth. partial plates are used when one or more natural teeth remain in the upper or lower jaw. not only does it fill in the spaces created by missing teeth, it prevents other teeth from changing position.
in general
new plates may feel a little odd or loose for a few weeks until the muscles of the cheeks and tongue learn to keep them in place and you get comfortable inserting and removing them. also, it is not unusual for minor irritation or soreness to occur and for saliva flow to increase when you first start wearing them, but these problems will diminish as the mouth adjusts
eating may be difficult initially. it will take a little practice and may be uncomfortable for some wearers for a few weeks. start with soft foods cut into small pieces. chew slowly using both sides of your mouth. as you get used to new dentures, add other foods until you return to a normal diet.
